The modern approach to wound treatment
Wounds have a variety of causes; some arise from surgical intervention, some are the result of injury, and others are a consequence of extrinsic factors, such as pressure or shear, or underlying conditions such as diabetes or vascular disease. They are often classified as a result of their underlying cause into acute wounds, such as surgical wounds and burns, and chronic wounds, such as leg ulcers, diabetic foot ulcers (DFUs) and pressure ulcers. Whatever the cause, wounds have a substantial but often unrecognized impact on those who suffer from them, on their carers and on the health care system. (1)
Good wound care is important because any wound is at risk of bacterial contamination, which inhibits the healing process and prevents wound closure. Non-healing wounds impact on mortality risk, patient function and quality of life. The resource impact on healthcare providers is equally important: a substantial proportion of acute hospital beds are occupied by patients with wounds (2) . Wound complications are associated with longer and more intensive treatment, extended hospital stays, readmission and specialist medical or surgical intervention.
The wound-healing process consists of four highly integrated and overlapping phases: hemostasis, inflammation, proliferation, and tissue remodeling or resolution. These phases and their biophysiological functions must occur in the proper sequence, at a specific time, and continue for a specific duration at an optimal intensity. There are many factors that can affect wound healing which interfere with one or more phases in this process, thus causing improper or impaired tissue repair.
In general terms, the factors that influence repair can be categorized into local and systemic. Local factors are those that directly influence the characteristics of the wound itself (low tissue oxygenation, infection, necrosis, etc), while systemic factors are the overall health or disease state of the individual that affect his or her ability to heal (age, diabetes, immunocompromised conditions etc). (3)
The modern approach to wound treatment implies a complex effect on systemic and local factors (4):
-
Cause-directed treatment - optimal, timely diagnosis and treatment of the wound cause.
-
Debridement - removes non-viable tissue, reduces the bacterial bioburden and the presence of biofilms, and leaves a clean surface that allows the migration of healthy cells into the wound (5).
-
Stimulation of tissue regeneration - electrical stimulation, magnetotherapy, cellular technologies to promote the wound closure.
Overcoming some systemic factors is a long-term issue, and some factors cannot be completely eliminated:
-
elderly age,
-
diabetes,
-
antibiotic resistant infection,
-
immunosuppressive therapy in oncological treatment or organ transplantation.
In this case, consistent measures to clean the wound, stimulate revascularization, granulation and epithelialization are key to avoid amputation and disability, successfully continue chemotherapy and radiotherapy, manage pain and the patient's quality of life.
We present a new laser method of wound treatment, which includes:
Laser demridement + Laser stimulation of regeneration
Laser debridement
Debridement plays a vital role in wound bed preparation and the removal of barriers that impair wound healing. Debridement helps remove nonviable tissue, control inflammation or infection, decrease excess moisture, and stimulate a non-advancing wound edge. (8)
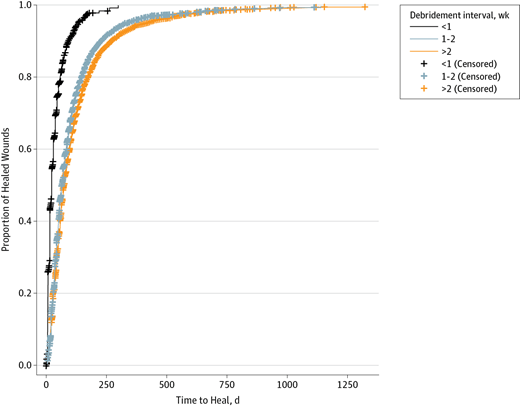
Wounds with debridement intervals of 1 week or less heales significantly faster.
Wilcox checked this in 2013. In a study of 154 644 patients with 312 744 wounds of all causes debridement were checked as a parameter. He found the following. The more frequent the debridements, the better the healing outcome. Although limited by retrospective data, this study’s strength was the analysis of the largest wound data set to date.
James R. Wilcox at al. Frequency of Debridements and Time to Heal. A Retrospective Cohort Study of 312 744 Wounds. JAMA Dermatol. 2013;149(9):1050-1058
There are many types of debridement, each with a set of advantages and disadvantages. (7)
| Debridement method | Advantages | Disadvantages |
|---|---|---|
| Autolytic |
|
|
| Chemical (proteolytic enzymes) |
|
|
| Mechanical |
|
|
| Surgical (sharp) |
|
|
| Biological (maggot therapy) |
|
|
| Ablative Er:YAG laser debridement |
|
|
Ablative Er:YAG laser debridement
Laser debridement is based on the controlled vaporization of the superficial layers of the wound bed. This results in the removal of the tissue containing unwanted microbial and necrotic particles.
The output laser parameters and the number of passes performed determine the depth of tissue ablation.
Advantages of laser debridement include precision and uniformity of tissue ablation, which reduces trauma to the wound bed, improving patient comfort.
By utilizing a short-pulsed system, laser energy is delivered in high-intensity, rapid succession pulses, resulting in short duration and high temperature exposure of target tissue, thereby minimizing thermal injury. (9)
The pulsed Er:YAG laser emits light within the mid-infrared portion of the electromagnetic spectrum with a wavelength of 2940 nm that corresponds to the absorption peak of water. The absorption coefficient of the Er:YAG is 12800 cm-1 whereas that of the CO2 laser is only 800 cm-1, rendering Er:YAG energy to be 12-18 times more efficiently absorbed by water-containing tissues. Because 90% of the soft tissue is composed of water, most of the Er:YAG energy is superficially absorbed.
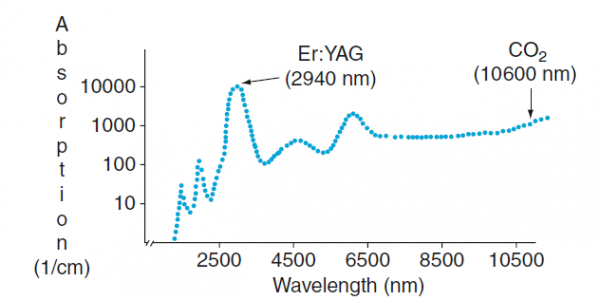
Fig.1 Water absorption coefficient graph
Each pass of the erbium heats tissue to over 300°C as a result water in the tissue is rapidly expanded to eject the charred debris from the wound surface without leaving behind a necrotic eschar (10).
The Er:YAG laser provides distinct advantages in precise ablation control and the reduction of residual necrotic tissue burden with minimal procedural discomfort, making the Er:YAG laser the most suitable device for laser wound debridement.
Laser stimulation RecoSMA™
The Essence of the method
Stimulation of reparative regeneration of cells and tissues through induced mechanical trauma.
Induction of mechanical damage to cellular structures
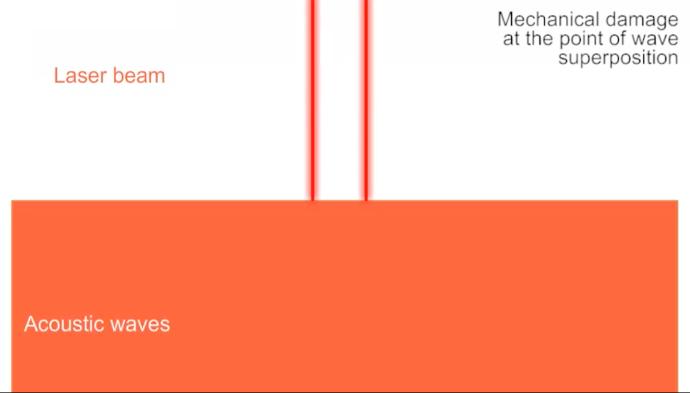
Absorption of a short laser pulse creates mechanical stress waves that propagates out of the laser irradiated site into the surrounding tissue. In case of simultaneous impact of several sources, multiple waves will be generated.
Using a special SMA module, the erbium laser radiation is divided into many microbeams, which together create a periodic structure of the stress wave epicenters on the surface of the irradiated tissue.
By changing the energy and duration of laser radiation pulses, it is possible to vary the power of these waves, thereby changing the depth and degree of microtrauma.
Pre-clinical studies
Method of cell damage due to mechanical impact.
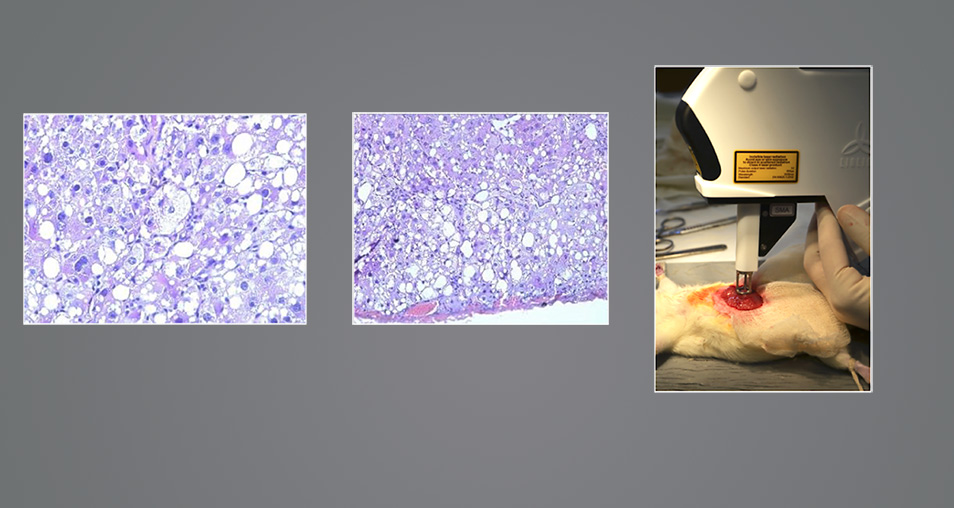
Preclinical studies of the effect of spatially modulated ablation on the intact skin of white rats showed the presence of multiple mechanical (non-thermal) lesions in the tissues with subsequent regeneration, without the formation of microfibrosis.
7th Joint Meeting of the European Tissue Repair Society & the Wound Healing Society (ETRS-WHS 2015), 21-23 October in Copenhagen, DenmarkThe Ability to Regenerate the Liver in Experimental Animals with Induced Cirrhosis under the Influence of the Spatially Modulated Erbium Laser.
In the experiment the liver cirrhosis was modeled in 70 albino outbred rats by means of carbon tetrachloride. Cirrhotically changed left liver lobe was treated by micro-ablation method (erbium laser, wavelength of 2,936 μm, impulse duration of 0,3 ms, packed with SMA (Spatially Modulated Ablation), the right lobe was a control one. The repeated operations with the treating of the liver have been carried out on the 15th, 30th, 60th days, followed by exclusion from the experiment and histological examination of the liver.
After a single treating of the rats’ liver with spatially modulated erbium laser radiation at microscopy on the first day of exposure the signs of pre-existing liver cirrhosis in the hepatic tissue so as on the depth of exposure (from 5,5 to 6,0 Mm) the destruction of some hepatocytes were revealed. Starting from the 30th day the regeneration signs of cirrhotically changed liver were established, including the reduction of the connective tissue amount and signs of the portal hypertension. At the same time no signs of regeneration in the right liver lobe not subjected to laser radiation were revealed. On the 60th day after double liver treating neoangiogenesis, proliferation of the bile ducts, reduction of the number of false lobules and connective tissue structures have been registered compared to the right lobe of the liver, which treating is not performed.
Conclusion: The impact of the micro-ablative method on the cirrhotically changed liver causes active process of regeneration that may be indicated for application Bridge-therapy prior to liver transplantation.
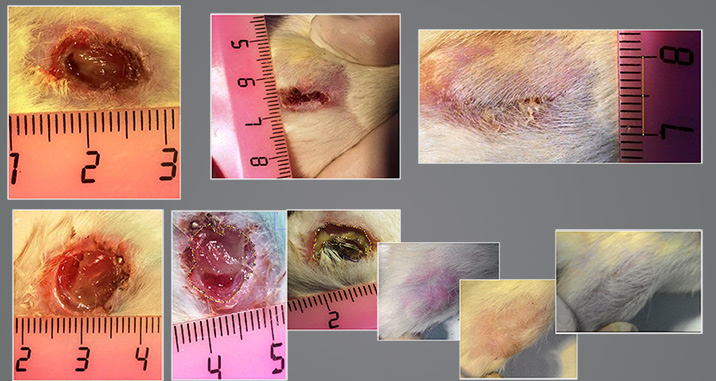
Experimental studies on white rats: treatment of neurotrophic ulcers.
The model for neurotrophic ulcers was formed by crossing the sciatic (femoral) nerve and forming a skin abnormality. Without the treatment, the defect didn’t heal while under observation for 1 month.
Using SMA treatment allowed us to close the defect within 2 weeks - with the formation of healthy and functional skin.
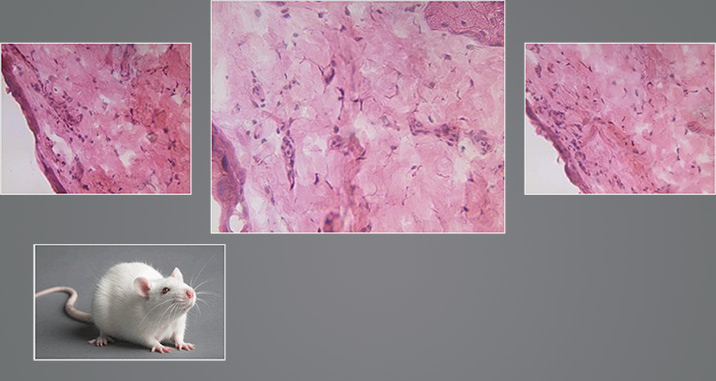
Experimental studies on white rats: treatment of burns.
The treatment of burn wounds while experimenting with this reparative stimulation method using SMA exposure allowed us to heal them in the same amount of time as with the control group (top line photo), but without course scaring, which was verified macro and microscopically (bottom line photo).
7th Joint Meeting of the European Tissue Repair Society & the Wound Healing Society (ETRS-WHS 2015), 21-23 October in Copenhagen, DenmarkProtocol for laser treatment of chronic wounds
Equipment and materials used
-
MULTILINE medical laser device complete with Er:YAG pulsed erbium laser and SMA module for spatial beam splitting.
-
Dressing.
Indications for use
-
Long-term non-healing wounds,
-
purulent wounds, including those with antibiotic-resistant microflora,
-
trophic ulcers of various etiologies.
Contraindications
Oncological diseases in the treatment area.
Technology of using the treatment method
The treatment method consists of 2 stages:
-
Debridement - wound cleansing from non-viable (necrotic) tissues, fibrin, plaque containing microflora (microbial biofilms).
An Er:YAG laser emitter is used with optical tips that form the working radiation spot size of 3 and 6 millimeters in diameter.
Laser radiation is directed to the wound surface and layer-by-layer evaporation of the wound contents is carried out under visual control, over the entire area, using a scanning method. The amount of tissue evaporated per pulse depends on the energy density. At the first stage of treatment, when it is required to remove the purulent contents of the wound and large volumes of necrotic tissues, it is recommended to use an energy density of 7-10 J/cm2. When approaching viable tissues, in order to avoid injury to the wound bed, it is recommended to reduce the energy density to 3 J/cm2. The criterion for the sufficiency of the first stage of processing is the visualization of healthy tissues and the appearance of capillary bleeding ("blood dew"). -
Stimulation of reparative processes in the wound to accelerate healing. An Er:YAG laser is used with an attached SMA module.
Processing is recommended to be performed by scanning the area of the cleaned wound bed and surfaces adjacent to the wound.Set Fluence between 2 and 4 J/cm2. The depth of impact depends on the value of the energy density, which increases with increasing fluence. At the same time, with an increase in energy density above 3 J/cm2, the area of surface ablation also increases, which can lead to an injured wound bed and wound edges.
The effectiveness of the impact also depends on the width of the treatment area around the wound. To obtain a good therapeutic effect, treatment of surrounding tissues is required at a distance of at least one centimeter from the edge of the wound. After the treatment session, the wound is closed with a dry aseptic dressing.A second session of wound treatment is performed a day after the previous treatment if the wound has purulent contents, non-viable tissues, signs of the presence of pathogenic flora. In this case, it is necessary to re-debride the wound bed (stage 1) and stimulate repair (stage 2). In the absence of purulent contents in the wound, non-viable tissues and signs of the presence of pathogenic flora, the debridement stage is not carried out.
For complete healing of the wound and its epithelialization or preparation for transplantation of the skin flap, several sessions of both debridement of the wound and stimulation of reparation may be required, the number of which is individual and depends both on the size of the defect and on its origin. It is recommended to increase the intervals between sessions from daily treatments to one session every 7-14 days.
Clinical case reports
State Institution "Minsk Scientific and Practical Center for Surgery, Transplantology and Hematology, Belarus
Dr. Ivan Pikirenia, Ph.D, Head of the Department of Transplantology, Associate Professor
As part of a clinical study of the laser treatment of chronic wounds, 204 patients were treated at the Minsk Scientific and Practical Center for Surgery, Transplantology and Hematology.
| Diseases and conditions | No. of patients |
|---|---|
| Trophic ulcers of the lower extremities | 97 |
| Pressure ulcers | 14 |
| Non-healing wounds of the anterior abdominal walls | 41 |
| Post-traumatic non-healing wounds | 9 |
| Diabetic foot | 10 |
| Non-healing wounds of other localizations and etiologies | 33 |
Trophic ulcers of the lower extremities
A total of 97 patients were treated. The age of the ulcer is from 3 months to 18 years.
There is a good effect of erbium laser radiation on trophic ulcers in patients with liver cirrhosis who are on the waiting list for liver transplantation. 3 patients with this pathology were successfully treated.
All the treatments where only Er:YAG laser + SMA-module (no drug therapy and no additional topical treatment).
Our observations have shown that laser debridement of the surface of trophic ulcers and stimulation of repair by SMA exposure can significantly reduce pain in the ukcers area and give up analgesics.
Diabetic wounds
- No antibiotics as elimination of pathogenic flora by laser debridement.
- Wound healing by tissue proliferation not by contraction
Non-healing surgical wounds
The use of laser debridement and laser stimulation of regeneration made it possible to successfully prepare non-healing wounds for resuturing in the following cases:
- liver and kidney transplant,
- pancreatic necrosis,
- acute intestinal obstruction,
- abdominoplasty,
- appendectomy,
- surgery followed by chemotherapy.
Amrut wound clinic, India
Dr. Dhirendrakumar Patil, MBBS, MS - General Surgery, MCh - Plastic Surgery Plastic Surgeon, Diabetic Foot Surgeon
We have been using Er:YAG RECO™ laser treatment for diabetic wounds for over 5 years.
RECO™ laser heals these wounds by stimulating regeneration of different tissues and heals these wounds in more efficient manner. RecoSMA™ laser by way of Neo-angiogenesis and proliferation of fibroblast and epithelium heals these wounds in more normal and natural way instead of wound contraction.
Treatment is done first with ablative mode to eliminate pathogenic bacterial flora and micro necrectomy to remove dead tissue in wound floor. Then in same session treatment is done with SMA tip to induce tissue regeneration. Due to process of tissue proliferation wound contraction does not happen. Thus deformities are avoided.
Normally diabetic wound patients are advised not to take weight on affected foot. Unlike this while treating these wounds with RecoSMA™ laser patient is advised to walk with full weight on affected foot. This helps in patient feeling psychologically better. Since wound heals with full weight bearing problem of wound recurring due to breakdown of fibrotic tissue later, does not happen.
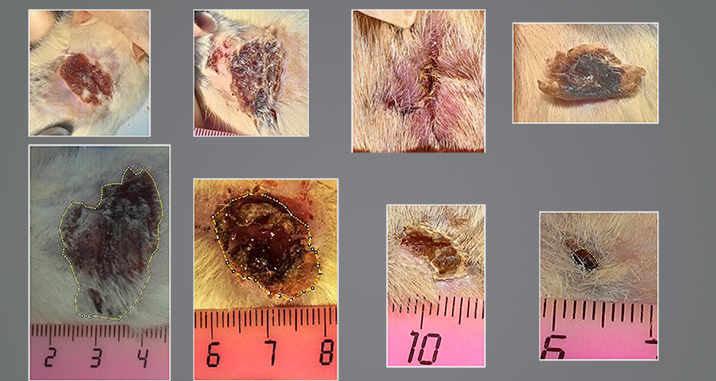
Patient1.Non-healing diabetic wound, 6 month old,
treatment Er:YAG laser + SMA-module,
Session - 8
Patient2.Non-healing diabetic wound, 6 month old,
treatment Er:YAG laser + SMA-module,
Session - 10
Elrevo Plastic Surgery Clinic, India
Dr. Ram Mahadev Chilgar, MBBS, MS - General Surgery, MCh - Plastic Surgery
Patient1. 45/m, Non healing wound 3 years old,
Co-morbidity – underlying osteomyelitis and over ankle joint,
treatment Er:YAG laser + SMA-module,
Session - 1
Patient2. 45/m, Venous ulcer 2 years old,
Co-morbidity – Diabetes, varicose veins and hypertension,
treatment Er:YAG laser + SMA-module,
Patient3.54/f, Non healing ulcer on thigh,
Co-morbidity – Patient on long standing steroid since 8 years due to arthritis,
treatment Er:YAG laser + SMA-module,
Session - 8
References
-
J. Posnett, F. Gottrup, H. Lundgren, G. Saal The resource impact of wounds on health-care providers in Europe. J Wound Care 2009; 18: 4, 154-161.
-
Mahe, E., Langlois, G.,Baron, G. et al. Results of a comprehensive hospital- based wound survey. J Wound Care 2006; 15: 9, 381-384.
-
S. Guo and L.A. DiPietro Factors Affecting Wound Healing. J Dent Res. 2010 Mar; 89(3): 219–229.
-
R. Gary Sibbald, James A. Elliott at al. Wound Bed Preparation 2021. Adv Skin Wound Care. 2021 Apr; 34(4): 183–195. (link)
-
Schultz GS, Sibbald RG, Falanga V et al (2003) Wound bed preparation: a systematic approach to wound management. Wound Repair Regen 11(Suppl1): S1-28
-
Wolcott RD, Kennedy JP, Dowd SE (2009) Regular debridement is the main tool for maintaining a health wound bed in most chronic. J Wound Care 18(2): 54-6
-
ANNA F. FALABELLA Debridement and wound bed preparation. Dermatologic Therapy, Vol. 19, 2006, 317–325
-
James R. Wilcox at al. Frequency of Debridements and Time to Heal. A Retrospective Cohort Study of 312 744 Wounds. JAMA Dermatol. 2013;149(9):1050-1058
-
Efficacy of Laser Debridement on Pain and Bacterial Load in Chronic Wounds. ClinicalTrials.gov Identifier: NCT03182582
-
Alster TS, Lupton JR. Erbium:YAG cutaneous laser resurfacing. Dermatol Clin. 2001 Jul;19(3):453-66.